This month I was lucky enough to hear David Kolesky from Harvard University’s Wyss Institute discuss his team’s latest work on 3D bioprinting. The idea that we are beginning to be able to print human tissue is mind-blowing, and to hear details from someone in the forefront of this work was awe-inspiring.
Human Tissue Engineering: Challenges and Solutions
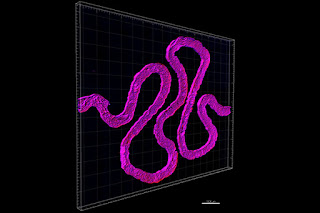
David Kolesky is part of a team at Jennifer Lewis' Research Group at the Harvard John A. Paulson School for Engineering and Applied Sciences (SEAS) and the Wyss Institute for Biologically Inspired Engineering at Harvard University who is working on engineering human tissue. In his talk at Biotech Week Boston on October 6, Kolesky focused on the team's work with engineering kidney tissue in particular. He described his team’s focus and some of their challenges: “(A human) kidney has a million nephrons, within the nephron we’re focused on the proximal tubule” and “(human) tissue is extremely difficult to mimic, because (of its) hierarchical structures that have a composite nature.” (You can see the tubule below, courtesy Wyss Institute.)
Stem-Cell Laden ‘Ink’ Becomes Living Tissue
Kolesky told the story of exactly how he was using 3D printing, specifically “bioprinting” to solve the challenges of vascularization. To someone not well versed in the latest discoveries it was fairly astounding – especially when he elucidated the use of “stem-cell laden ‘ink’ to build fully vascularized human tissue”. The materials they’re using are almost as fascinating at the engineered tissue: a hydrogel, which becomes “liquid when cooled” is the substance Kolesky and the Wyss Institute is using to make the bioprinting happen. With the methods he’s using, they are able to “keep these vascular networks perfusable for up to 45 days”. Their 3D printed proximal tubules actually contain living human cells and mimic many biological functions of nephrons.
How do they do that? Once the tubules are printed, they pump living kidney cells into them. After several days in the tubules the cells begin to function like the ones in our bodies. Cells in the tubules are “trained” by the chemistry of their environment to become and behave exactly like native kidney cells.
Researchers Can Now Study Real-Time Damage To Tubules
There are 60,000 people on a national waiting list for kidneys, and the CDC says that 1 in 10 American adults, more than 20 million people, have some level of chronic kidney disease. There is an urgent need for science to advance this research. The Wyss Institute is not only at the forefront of bringing us closer being able to engineer human kidneys in the future; with the current research researchers will actually be able to induce damage on these bioengineered tubules as if they were the real thing to study effects of drugs or toxins.
We Want a Synergistic Relationship with Biology
Kolesky closed his talk with the quote: ”We want a synergistic relationship with biology.” In fact Wyss Institute's Mission Statement is: "The Wyss Institute seeks to transform engineering, medicine and the environment by creating new materials and devices using Nature’s design principles".
Their team's paper:”Bioprinting of 3D Convoluted Renal Proximal Tubules on Perfusable Chips” was published in Nature Scientific Reports several days after Biotech Week Boston and gives more detail on Kolesky’s research. You can read the paper here.
Interested in hearing more about innovations in the intersection of bioengineering and medicine? Download our report here. And don't forget to follow Biotech Week Boston on Twitter for news on innovation in biotech and medicine. Each year passionate scientists and innovators converge on Boston to share ground breaking data, research and ideas - don't miss our next event in September 2017!
|
Share this article with your social network, just click below to share now!
|
|
|












No comments :
Post a Comment